Scoliosis is a complex three-dimensional deformity affecting the spine and the trunk. It occurs in functional and possible structural changes in the three planes of the body and could be defined as a three-dimensional torsional deformity. (Grivas2006)
The word “scoliosis” comes from the Greek for “crooked” (scolios). (Vasiladis2009)
Scoliosis or idiopathic scoliosis affects mostly children and adolescents during the growth spurt. The causing factor is described as multifactorial with genetic, hormonal, muscle-skeletal, neurological components, and was put together in various theories. (Burwell 2003, 2006,2013,2016)
Idiopathic scoliosis can be subdivided according to the time of detection:
| Infantile Idiopatic scoliosis |
(IIS) | age 0 – 3 | more boys, thoracic left, thoracic kyphosis |
| Juvenile Idiopatic scoliosis |
(JIS) | age 4 – 9 | Typical features: more girls, thoracic right-convex, lumbar left-convex, risk of respiratory dysfunction, flatback early onset <10J (SRS-Definition) |
| Adolescent Idiopatic scoliosis |
(AIS) | age >9 – 17 | see JIS late onset >10J |
Adult idiopathic scoliosis and degenerative scoliosis
A new group of more or less idiopathic scoliosis is adult scoliosis. It occurs a long time after skeletal maturity, and stable curvature has been reached and is in a sense the “restart” or renewal of progression.
The degenerative scoliosis starts in the post-menopause (age 50-60yr) (de novo – new) accompanied with LBP (low back pain) even in mild curves, LL (Lateral Olisthesis) in more severe curves, segmental instability, osteopenia or osteoporosis and loss of lumbar lordosis. Woman especially in the lumbar area are more affected.
It could be explained as a lack of compensatory options because of the reduced flexibility to compensate with secondary curvatures and the loss of postural stability especially in the sensible lumbar-pelvic area.
Degenerative lumbar scoliosis has a high risk of further progression und is reducing health related quality of life because of the pain and functional impairments.
Aebli M, The adult scoliosis, EurSpineJ (2005)
Scoliosis with a known etiology is described as congenital (vertebral bone defects or irregular segmentation from birth on), neuromuscular (defects in the neuro-motor system), or scoliosis according to different systemic diseases. (see below)
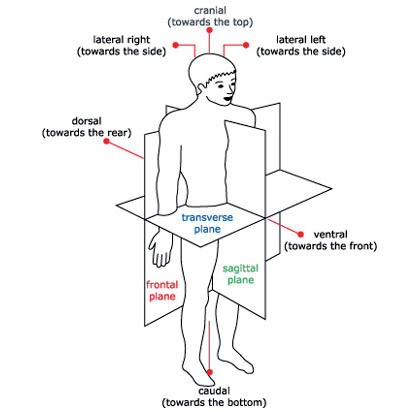
Scoliosis viewed in the frontal plane exhibits a lateral deviation. In the transverse plane, axial rotation of the vertebrae is observed mostly around the apex of the curvatures, combined with torsion in the same vertebral segments. In the sagittal plane, the physiological curves (kyphosis thoracic and lordosis lumbar) tend to become reduced in the direction of a thoracic flatback the lumbar lordosis seems more variable depending on the curve type. Typical changes in the sagittal plane are described for the thoracolumbar junction. (Schlösser2014)
Truncal features in scoliosis generate an asymmetric body relief due to the rotational aspects with dorsal expansions on the convex side of the curvatures and indented areas corresponding to the concavities. The frontal and sagittal balance depends on the compensatory effects of primary and secondary curvatures.
The gold standard for the scoliosis diagnosis ist still an ap x-ray film in an upright position detecting lateral deviation and defines according to the SRS (scoliosis research society) standards scoliosis with a Cobb angle more than 10° with axial rotation.
Curvatures are limited by an upper-end vertebra and a lower-end vertebra with an apex (apical vertebra) in the center of the curve. At the apical vertebra, the spinal rotation could be assessed with different methods, Nash & Moe, Pertriolle, Raimondi.
In the clinical assessment measurement with the Bunnel scoliometer reports the angle of trunk rotation. Values more than 5° or 7° respectively indicate further investigation.
A distinction is made between structural scoliosis and functional scoliosis. Functional scoliosis is mainly seen in cases of postural damage, or secondary to extraspinal causes, e.g. different leg lengths paraspinal muscle asymmetry. In such cases, the scoliosis is not fixed and can be adjusted in a reclined position or by the correction of the underlying causing factor.
Structural scoliosis features are typical components when the diagnosis scoliosis is reported and are clear signs for scoliosis progression increasing the Cobb angle, rotation, and rigidity in typical parts of the spine.
The structural fixation affects different tissues like bones, connective tissues, ligaments, muscles, etc, and is an expression of scoliosis due to the asymmetric loading on the growing and developing body system with its muscle-skeletal and locomotor components.
Body planes and directional terms
Scoliosis

Congenital scoliosis
Congenital scoliosis is a spinal deformity with lateral deviation and rotation of the spinal column caused by birth defects in the embryonal development of the vertebrae leading to the formation of one or more deformed vertebrae. The incomplete formation of the vertebrae results in asymmetrical growth of the spinal column. Congenitally anomalous vertebrae can occur in any part of the spinal column. Formation defects, segmentation defects, or combined forms of vertebral anomalies disturb the normal growth pattern of the spinal column, so that a scoliosis may develop as the spinal column develops. Congenital scolioses are rare, but may require early surgery due to the severity of the spinal deformity.
Neuromuscular scoliosis
This term describes a clinical picture resulting primarily from neurological or muscular diseases and characterized by a wide variety of symptoms of varying degrees of severity (for example disorders affecting posture and the locomotor system, mental disability, or damage to sensory perception functions). Many of these diseases have their onset in childhood and may, in addition to the many individual primary symptoms observed, also lead to the formation of a scoliosis due to the neuromuscular disturbance of the postural apparatus with local or generalized muscular dysfunctions.
(Harms, 2007)